ECGs in Acute Myocardial Infarction
Diagnosing an acute myocardial infarction by ECG is an important skill for healthcare professionals, mostly because of the stakes involved for the patient. One of the complications with using ECG for myocardial infarction diagnosis is that it is sometimes difficult to determine which changes are new and which are old. For the purposes of this learning module, we will assume that all changes are new for the patient and thus represent an acute myocardial infarction.
Acute Coronary Syndrome
An acute coronary syndrome may include various clinical entities that involve some sort of ischemia or infarction. Specifically, an acute coronary syndrome includes unstable angina, non-ST segment elevation myocardial infarction, and ST segment elevation myocardial infarction (STEMI). Occasionally, non-ST segment elevation myocardial infarction is referred to as non-Q wave myocardial infarction and STEMI is referred to as Q wave myocardial infarction. This is because ST segment elevation myocardial infarction is almost always associated with a pathological Q wave.
Myocardial Infarction
In order for a patient to be diagnosed with a myocardial infarction, they must have at least two of the following three criteria, according to the World Health Organization:
- Clinical history of chest discomfort consistent with ischemia, such as crushing chest pain
- An elevation of cardiac markers in blood (Troponin-I, CK-MB, Myoglobin)
- Characteristic changes on electrocardiographic tracings taken serially
As to the last point, comparing the patient’s current ECG with an old ECG is an important part of diagnosis. On the other hand, particularly worrisome changes by ECG should still be treated presumptively if the prior ECG is not available.
Pathological Q Waves
A pathological Q wave is a Q wave that is more than 0.04 seconds in duration and more than 25% of the size of the following R waves in that lead (except for leads III and aVR). Because pathological Q waves may take hours to develop and can last for a long time, the presence of new pathological Q waves indicates acute myocardial infarction but the mere presence of Q waves does not necessarily mean that a new myocardial infarction is taking place.
ST Segment Changes
One of the most significant findings of myocardial infarction is the presence of ST segment elevation. The ST segment is the part of the ECG tracing that starts at the end of the S wave and ends at the beginning of the T wave. The point where the end of the Q wave and the ST segment meet is called the J point. If the J point is greater than 2 mm above the baseline, it is consistent with an ST segment elevation myocardial infarction.
In the acute phase of non-ST segment elevation myocardial infarction, the ST segment may actually be depressed in leads that face the compromised portion of the heart. It is not possible to diagnose a non-ST segment elevation myocardial infarction by ECG alone. Patients are treated presumptively and diagnosis is made if the level of serum cardiac markers rise over several hours.
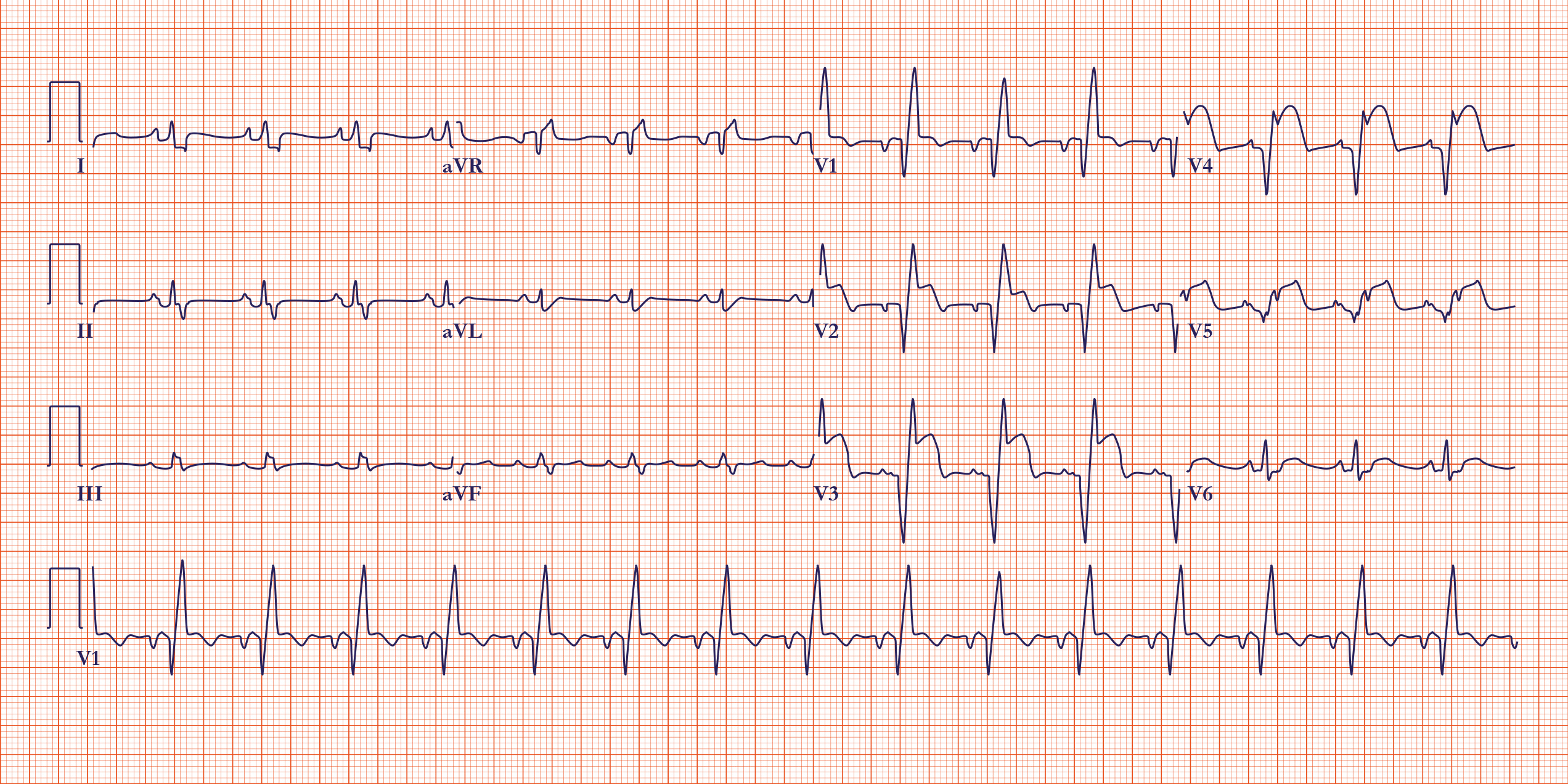
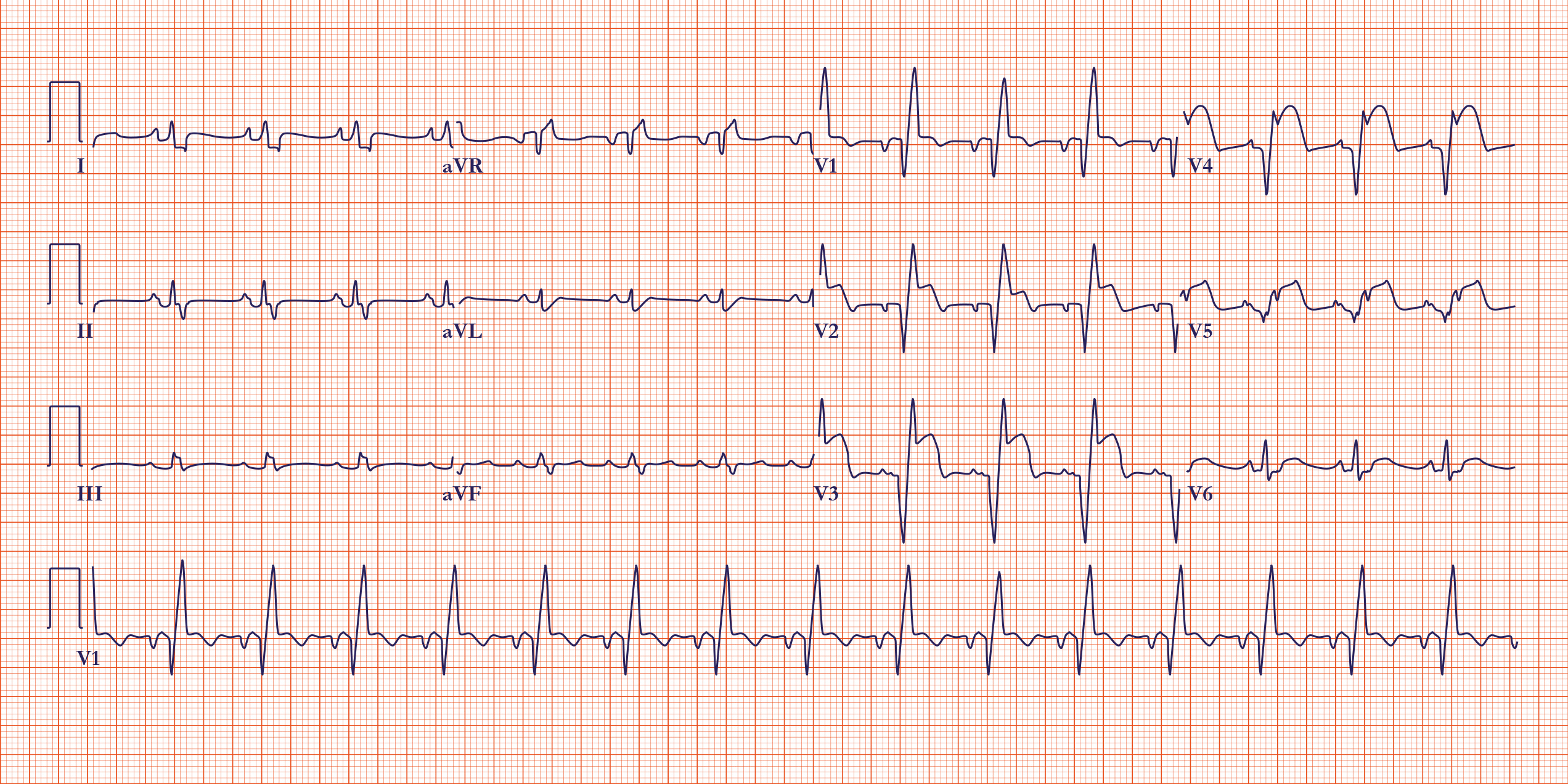
An example of an ST-segment elevation myocardial infarction
Where is the ischemic lesion?
A 12-lead ECG can be used to determine the coronary artery that is most likely affected by an ischemic event. Leads II, III, and aVF provide a view of the right coronary artery, for example. Primary changes on ECG involving these three leads suggests a problem in the right coronary. On the other hand, leads I, aVL, and V1 through V6 provide information about the left coronary artery.
Experienced users can analyze the ECG tracing to localize damage to specific areas of the heart. The inferior wall of the heart is likely compromised when there are active changes in leads II, III, and aVF. Abnormalities in leads V3 and V4 are suggestive of a problem in the anterior wall of the heart. Leads V1 and V2 provide information about the cardiac septum.
For each set of active changes e.g., J point elevation, there will be reciprocal changes in the complementary leads, which are opposite the affected area. For example, an active change in leads V3 and V4, suggesting a problem in the left anterior descending artery and affecting the ventricular septum, would be expected to cause reciprocal changes in leads II, III, and aVF.
ECG Changes during Myocardial Infarction (MI)
| Location of MI | Leads Affected | Vessel Involved | ECG Changes |
| Anterior wall | V2 to V4 | Left Anterior Descending artery (LAD) – Diagonal branch |
|
| Septal wall | V1 and V2 | Left Anterior Descending artery (LAD) – Septal branch |
|
| Lateral wall | I, aVL, V5, V6 | Left Coronary Artery (LCA) – Circumflex branch |
|
| Inferior wall | II, III, aVF | Right Coronary Artery (RCA) – Posterior descending branch |
|
| Posterior wall | V1 to V4 | Left Coronary Artery (LCA) – Circumflex branch Right Coronary Artery (RCA) |
|