EMS (with physician on board) is dispatched to a 42-year-old male with a chief complaint of chest pain and “possible heart attack.”
The patient is found lying on the couch. He appears to be reasonably comfortable and indicates that “the pain has eased a bit” since EMS was contacted.
While the patient is being undressed and the monitoring leads are attached a quick and focused history is obtained using the “SOCRATES” mnemonic.
- Site: Retrosternal
- Onset: The pain started about 1 hour ago while folk dancing at a party and become progressively worse over about 10 minutes
- Character: Poorly localized “tightness” or “discomfort”
- Radiation: Both arms and back
- Alleviating factors: Nothing makes the pain feel better
- Timing: The pain is persistent and follows no pattern
- Exacerbating: The pain seemed worse while walking to his car
- Severity: 8/10
The patient is diaphoretic but it is not clear whether it is from dancing or related specifically to the chest discomfort. He denies nausea, vomiting, palpitations, or shortness of breath, and states that he has not collapsed.
Social history: Smoking (40 pack years) and liberal alcohol use
Medical history: Hypertension
Medications: Unknown antihypertensive
Allergies: NKDA
Vital signs:
- RR: 16
- HR: 84
- NIBP: 125/82
- Temp:
- SpO2: 98% on room air
Physical exam:
The patient is a slightly overweight, stocky male, in no apparent distress. Mentation and speech are normal. Respirations appear normal. Breath sounds are clear bilaterally. Abdomen is soft and non-tender. No JVD or pitting edema. Strong radial pulses are noted bilaterally.
With this focused history and physical, acute coronary syndrome (ACS) is highest on list of differential diagnosis, with pulmonary embolism (PE) and aortic dissection possible, but much lower on the list.
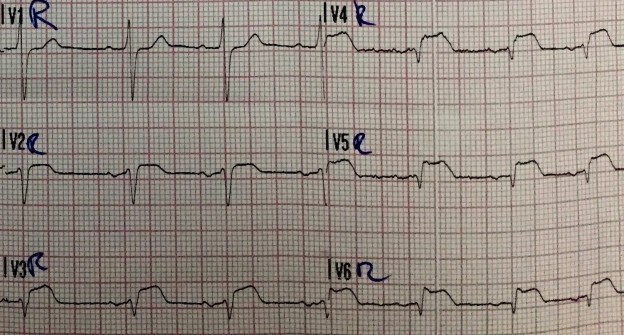
A 12-lead ECG is obtained.
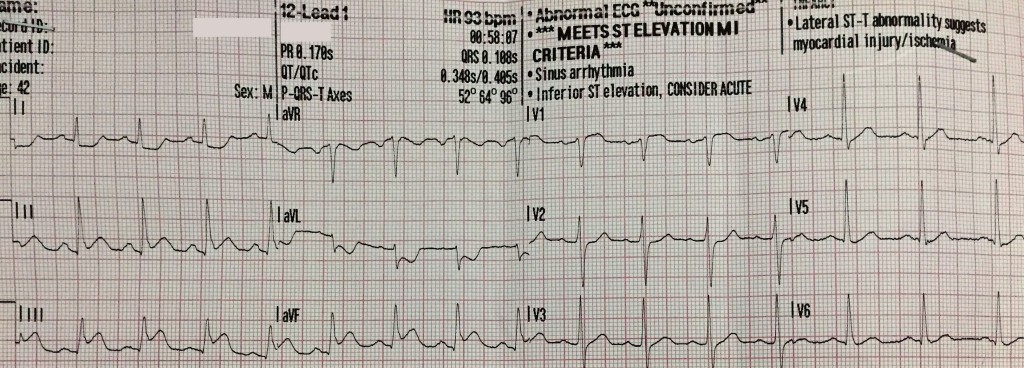
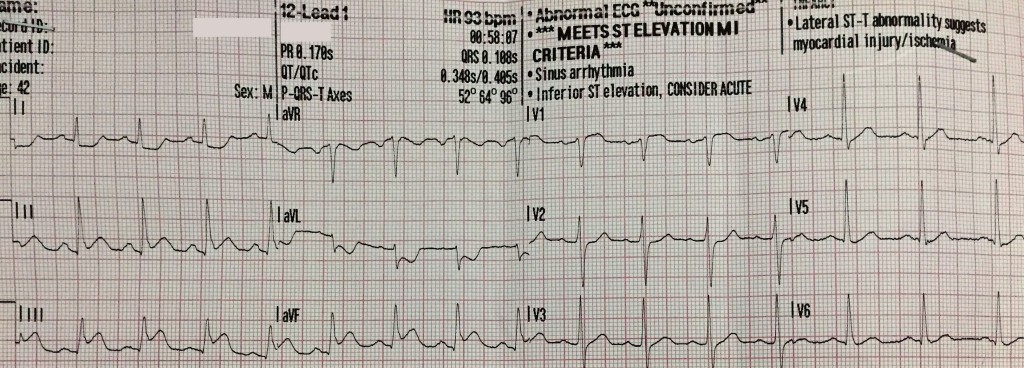
ST-segment elevation is noted in leads II, III, and aVF with reciprocal changes in leads I and aVL. STE III > STE II suggests occlusion of the right coronary artery (RCA) which suggests the possibility of RV infarction. Of note, there is a small amount of ST-segment elevation in lead V1 (also suggestive of RV infarction).
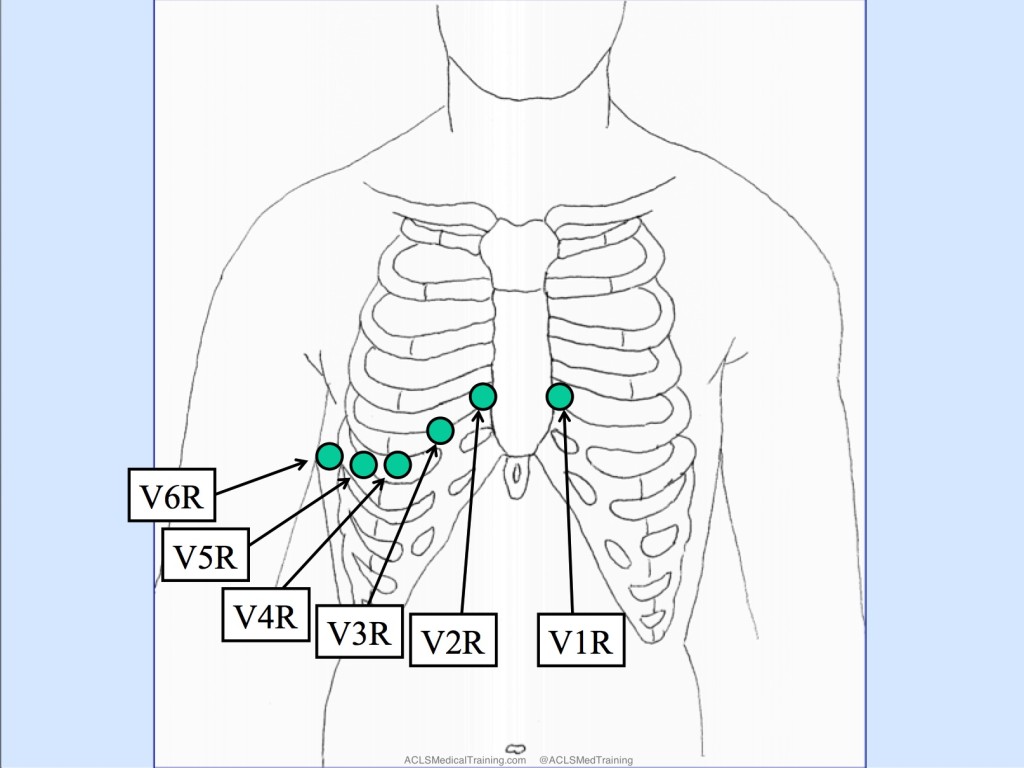
A right-sided 12-lead ECG is obtained. To accomplish this, the EMS crew places the precordial leads in the mirror-image position on the right side of the patient’s chest.
Editor’s note: Sometimes leads V1 and V2 are left in place and only leads V3-V6 are moved over to mirror image position on the patient’s right side.
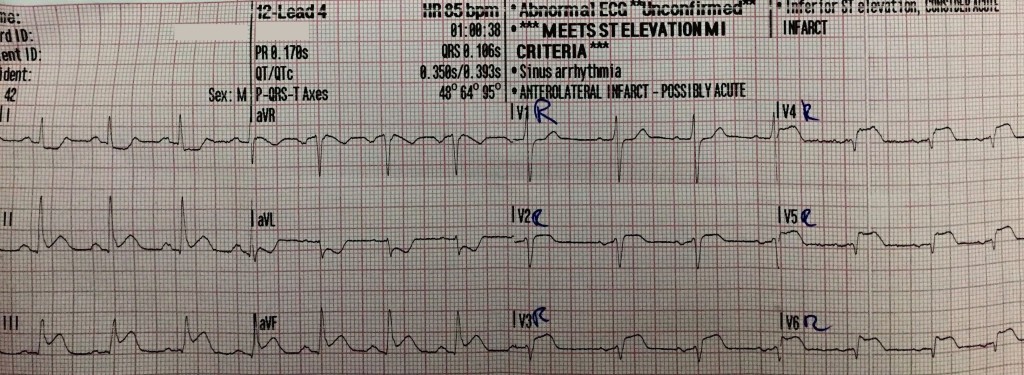
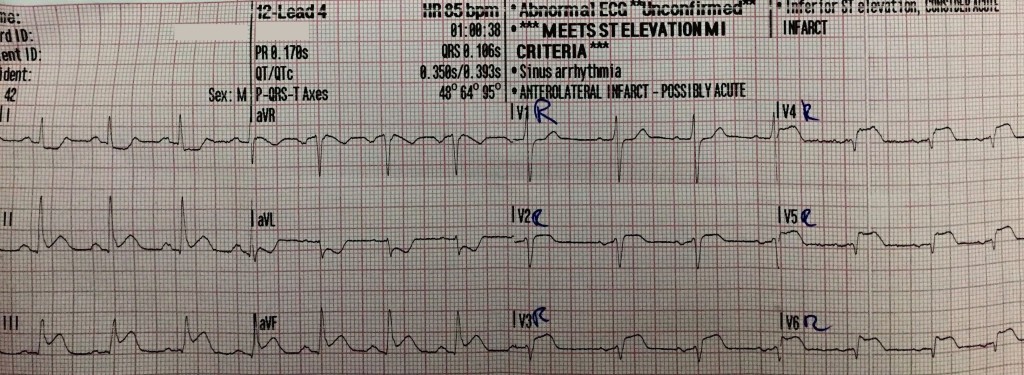
ST-segment elevation is noted in leads V2R, V3R, V4R, V5R, and V6R suggesting proximal occlusion of the RCA and right ventricular infarction.
Prehospital treatment:
- Aspirin 250mg PO
- Ringers lactate 500 ml
- 50 mcg of Fentanyl
- Oxygen was not given as the patient reported and presented no signs of dyspnea
- A trial dose (0.4 mg) NTG SL was given as RV infarction is a (relative) contraindication
The local receiving hospital and PCI unit are contacted by cell phone and the cardiac cath lab is activated.
Additional anticoagulant and antiplatelet therapy is given in the field.
- Heparin 5000 units IV
- Prasugrel 60 mg PO
The 15-minute ride to the PCI center is uneventful and patient’s symptoms improve.
The local ED team is notified of patient’s arrival and the transfer goes smoothly. The ED physician even exchanges a “high five” with the EMS crew.
As the prehospital physician is finishing his paperwork and discussing details of the case with the receiving physician, the nurses call for help. The team rushes into the resuscitation room to find the patient unresponsive with VF on the monitor.
CPR is initiated and the patient is defibrillated a total of 3 times. After the 3rd shock the patient erupts into wild seizure-like activity and lets out a scream followed by wild, deep inspirations.
The monitor shows a perfusing rhythm with a strong carotid pulse. The patient wakes up and asks, “What just happened?”
The patient is whisked away to the cardiac cath lab where a 95% occlusion to the RCA is successfully opened and stented. The patient is discharged a few days later.
Take-away points:
- Know your differentials and obtain a swift, focused history (SOCRATES is a useful checklist)
- All patients with chest pain should receive a 12-lead ECG early in the patient encounter
- When the patient is suffering acute inferior STEMI a right-sided 12-lead ECG can help to identify right ventricular infarction
- Be careful with nitroglycerin in the setting of right ventricular infarction
- STEMI patients should be monitored continuously with defibrillation pads in place.
- Don’t let your guard down! As Napoleon warned centuries ago, “The moment of greatest vulnerability is the instant immediately after victory.”
References:
1. https://en.wikipedia.org/wiki/SOCRATES_(pain_assessment)
2. Akbar A et al: Does this patient have an AMI? JAMA 1998;280(14):1256-63
3. Morris F, Brady WJ. ABC of clinical electrocardiography: Acute myocardial infarction-Part I. BMJ. 2002; 324: 831-4
4. http://emcrit.org/podcasts/emcrit-book-club-on-combat-by-grossman