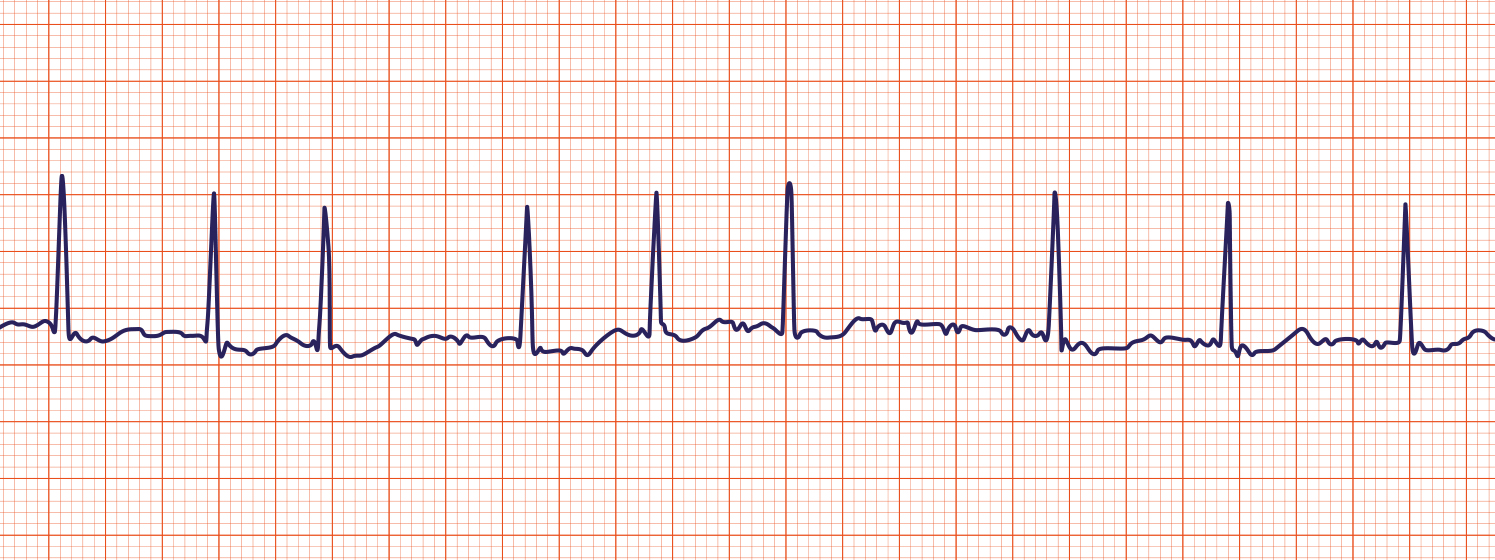
Atrial Fibrillation
Atrial fibrillation is the most common cardiac arrhythmia. The pulse of the patient experiencing atrial fibrillation is said to be “irregularly irregular” meaning that the pulse does not repeat in any discernible way. On an electrocardiogram, atrial fibrillation is the absence of distinct P waves. By contrast, atrial flutter appears on ECG as a sawtooth pattern. While it is difficult to quantify, the atrial contraction rate may exceed 300 bpm.
Atrial fibrillation can reduce cardiac output, since the atria are not contributing to ventricular filling. Instead, blood tends to stagnate or even coagulate inside of the atrium. This coagulation can be a problem because it can lead to thrombus formation, particularly in the atrial appendage. Once a thrombus forms, it can break apart and send emboli throughout the vasculature, perhaps to the lungs or the brain depending on which side of the heart is affected.
Symptoms
Atrial fibrillation can cause a number of symptoms or it may cause few symptoms at all. Patients will often report feeling chest palpitations, feeling as if their heart is racing, fatigue, dizziness or lightheadedness, weakness, and perhaps shortness of breath. In severe cases, atrial fibrillation may cause severe shortness of breath (dyspnea), chest pain (angina), low blood pressure (hypotension), or pre-syncope (dizziness, about to pass out). In rare instances, atrial fibrillation may prompt myocardial infarction (heart attack), syncope (passing out), or pulmonary edema (fluid in the lungs). Rarely, atrial fibrillation will be detected in a routine electrocardiogram or ECG performed for some other purpose.
Management of new onset atrial fibrillation
Is cardioversion needed?
If you encounter a patient with atrial fibrillation for the first time, the most important question you can ask is “does this patient need immediate cardioversion?” Cardioversion is the use of an electrical impulse applied to the chest to convert the atria back into a normal rhythm. Generally speaking, there are four indications for urgent cardioversion:
- Ischemia (lack of blood flow through the coronary arteries; myocardial infarction)
- Organ hypoperfusion (lack of blood flow to the organs; decreased urine output due to reduced blood flow to the kidney, for example)
- Congestive heart failure
- A preexcitation syndrome by electrocardiogram (rhythm that could switch to ventricular fibrillation or ventricular tachycardia without warning)
If any of these situations exist, then you should seek to use cardioversion immediately. In fact, this is more important than waiting to use anticoagulants before cardioversion. If possible, the patient should receive a bolus of heparin prior to emergent cardioversion, though this should not delay cardioversion. When cardioversion is not possible, one may consider using ibutilide, procainamide, or sotalol intravenously. Flecainide can be considered if the atrial fibrillation has been occurring for less than 24 hours and the patient does not have contraindications (e.g. structural heart disease, coronary artery disease).
When none of the four indications exist, then it is most often better to wait for appropriate anticoagulation before attempting cardioversion. This is especially true if the abnormal cardiac rhythm has been occurring for 48 hours or more, because the chance of thrombus increases significantly.
How do I control the rate?
If there is no evidence of heart failure (e.g., no pulmonary edema by chest x-ray; no “crackles” on lung exam) then the drugs of choice are beta-blockers or calcium channel blockers. If patients are experiencing heart failure, or if the atrial fibrillation is due to heart failure, then patients may be given digoxin.
How do I anticoagulate?
In a hospital or emergency department setting, the most common initial anticoagulant used is either low molecular weight or unfractionated heparin. This is given first as a bolus followed by a continuous intravenous drip. This can be transitioned to oral warfarin for outpatient management. Alternatively, patients can be transitioned to a non-warfarin oral anticoagulant such as dabigatran or apixaban. In most cases (non-emergent situations), patients should be sufficiently anticoagulated before cardioversion. It may take several weeks for the blood to be sufficiently anticoagulated.
If a transesophageal echocardiogram shows that there is no thrombus in the heart, patients may be proceeded to cardioversion. If the onset of atrial fibrillation can be determined definitively and the start was less than 48 hours before presentation, patients may not need anti-coagulation before cardioversion.
Note: The above describes the management of initial onset atrial fibrillation. The management of chronic atrial fibrillation differs substantially.