Fibrinolytic checklist
Professionals who provide emergency medical services may be called upon to administer prehospital fibrinolysis at some point in their careers. This is because several studies have shown that fibrinolytic agents given to people who are suffering from an acute cardiac event have better outcomes if they receive fibrinolysis (a clot-busting drug) before they reached the hospital. This is especially true in rural settings where the time to reach a hospital can be substantial. However, this may also apply in urban settings where wait times in emergency departments can be equally substantial.
Fibrinolysis can be effective for the treatment of ST-segment elevation myocardial infarction. The medication can dissolve the thrombus/embolus that is lodged in a coronary artery, thus restoring blood flow to the heart. Because of the possibility of serious adverse events, including serious bleeding events such as intracranial hemorrhage, the decision to administer fibrinolysis should not be entered into lightly. Anyone who is going to administer a clot-busting drug must be qualified to do so (including knowledge of ECG interpretation) and must only do so in patients who meet certain criteria.
Who may need prehospital fibrinolysis?
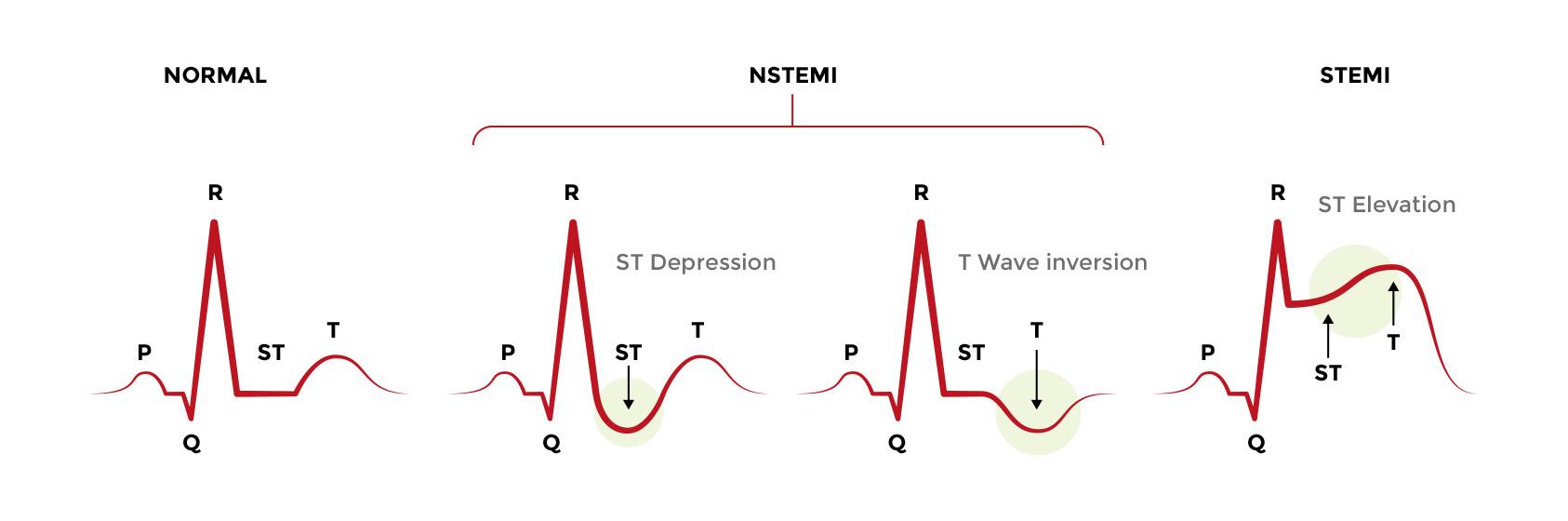
An ST-segment elevation myocardial infarction can be diagnosed using a 12-lead ECG obtained prior to reaching the hospital (in a patient with myocardial infarction symptoms such as crushing chest pain, for example). As the name implies, the ECG tracing shows an elevation between S and T waves. Roughly speaking, this means that the QRS complex connects to the T wave. Colloquially, clinicians refer to this as a “tombstone” because of its periods and what it used to mean for patients. In specific terms, an ECG that shows ST segment elevation in which the J point is greater than 2 mm in leads V2 and V3 and 1 mm or more in other leads is in ST segment elevation myocardial infarction. Likewise, a new or a likely new left bundle branch block may also receive fibrinolysis (See ECGs in Acute Myocardial Infarction).
Many electrocardiograms will include software that analyzes the ECG waveform and help direct users in making a diagnosis. However, given the seriousness of fibrinolysis, emergency medical services personnel (or anyone about to administer a fibrinolytic agent, for that matter) should be able to read the ECG independent from a software rating.
Absolute contraindications
If any of these factors exist, you should NOT administer a fibrinolytic agent1:
- History of any intracranial hemorrhage
- History of ischemic stroke within the preceding three months (unless it is an acute ischemic stroke occurring within the last three hours, then fibrinolysis is useful!)
- Presence of a cerebral vascular malformation or a primary or metastatic intracranial malignancy
- Symptoms or signs suggestive of an aortic dissection
- A bleeding diathesis or active bleeding, (menstruation is an exception)
- Significant closed-head or facial trauma within the preceding three months.
Relative contraindications
If any of these factors exist, you should consider NOT administering a fibrinolytic agent1:
- Severe hypertension or uncontrolled hypertension (blood pressure >180 mm Hg systolic and/or >110 mm Hg diastolic
- Ischemic stroke longer than three months ago
- Dementia
- Any known intracranial disease that is not an absolute contraindication
- If cardiopulmonary resuscitation was administered for >10 min
- Major surgery within the last three weeks
- Internal bleeding within the last two to four weeks
- Vascular punctures that could not be compressed if they were to start bleeding
- Pregnancy
- Currently on warfarin therapy
- Any allergic reaction to fibrinolytic drugs in the past
Good intravenous access and continuous cardiac monitoring should be instituted before fibrinolysis is given.
Prehospital Fibrinolytic Checklist*
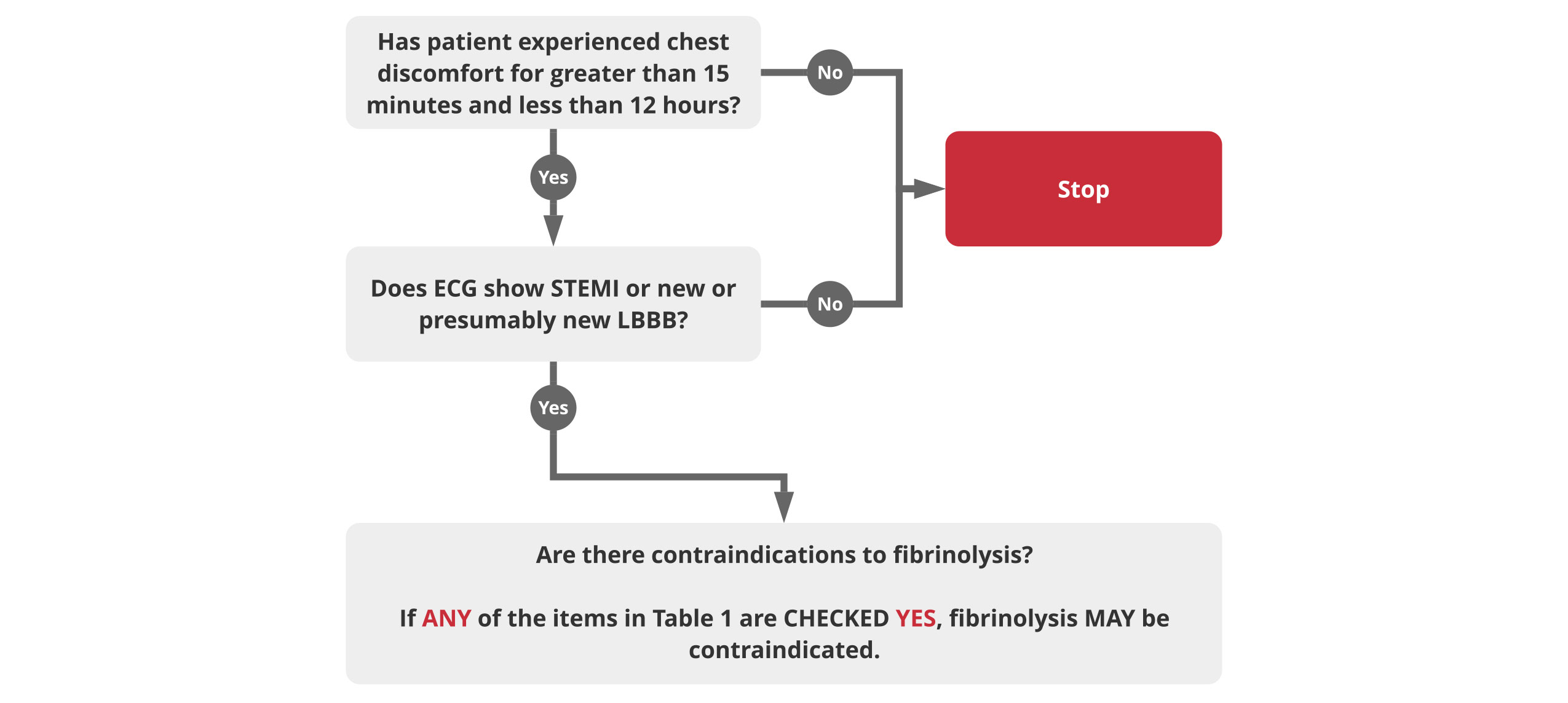
| Checklist | Yes | No |
| Systolic BP >180 to 200 mm Hg or diastolic BP >100 to 110 mm Hg | ||
| Right vs left arm systolic BP difference > 15 mm Hg | ||
| History of structural central nervous system disease | ||
| Significant closed head/facial trauma within the previous 3 months | ||
| Stroke >3 hours or <3 months | ||
| Recent (within 2-4 weeks) major trauma, surgery (including laser eye surgery), GI/GU bleed | ||
| Any history of intracranial hemorrhage | ||
| Bleeding, clotting problem, or blood thinners | ||
| Pregnant female | ||
| Serious systemic disease (eg, advanced cancer, severe liver or kidney disease) |
Table 1
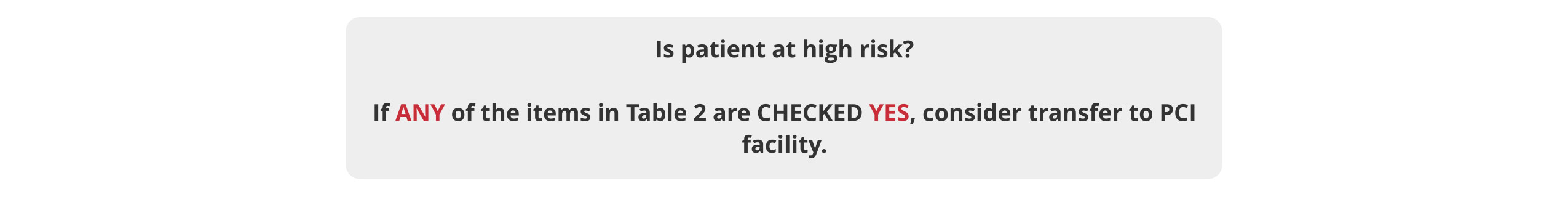
| Checklist | Yes | No |
| Heart rate >=100/min AND systolic BP <100 mm Hg | ||
| Pulmonary edema (rales) | ||
| Signs of shock (cool, clammy) | ||
| Contraindications to fibrinolytic therapy | ✝ | |
| Required CPR |
Table 2
* Contraindications for fibrinolytic use in STEMI are viewed as advisory for clinical decision making and may not be all-inclusive or definitive. These contraindications are consistent with the 2004 ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial infarction.
✝ Consider transport to primary PCI facility as destination hospital.
Prehospital fibrinolysis can significantly improve survival rates when treating acute myocardial infarction. Build the knowledge and clinical judgment to recognize candidates and administer care safely with our ACLS certification program.