Quantitative Waveform Capnography
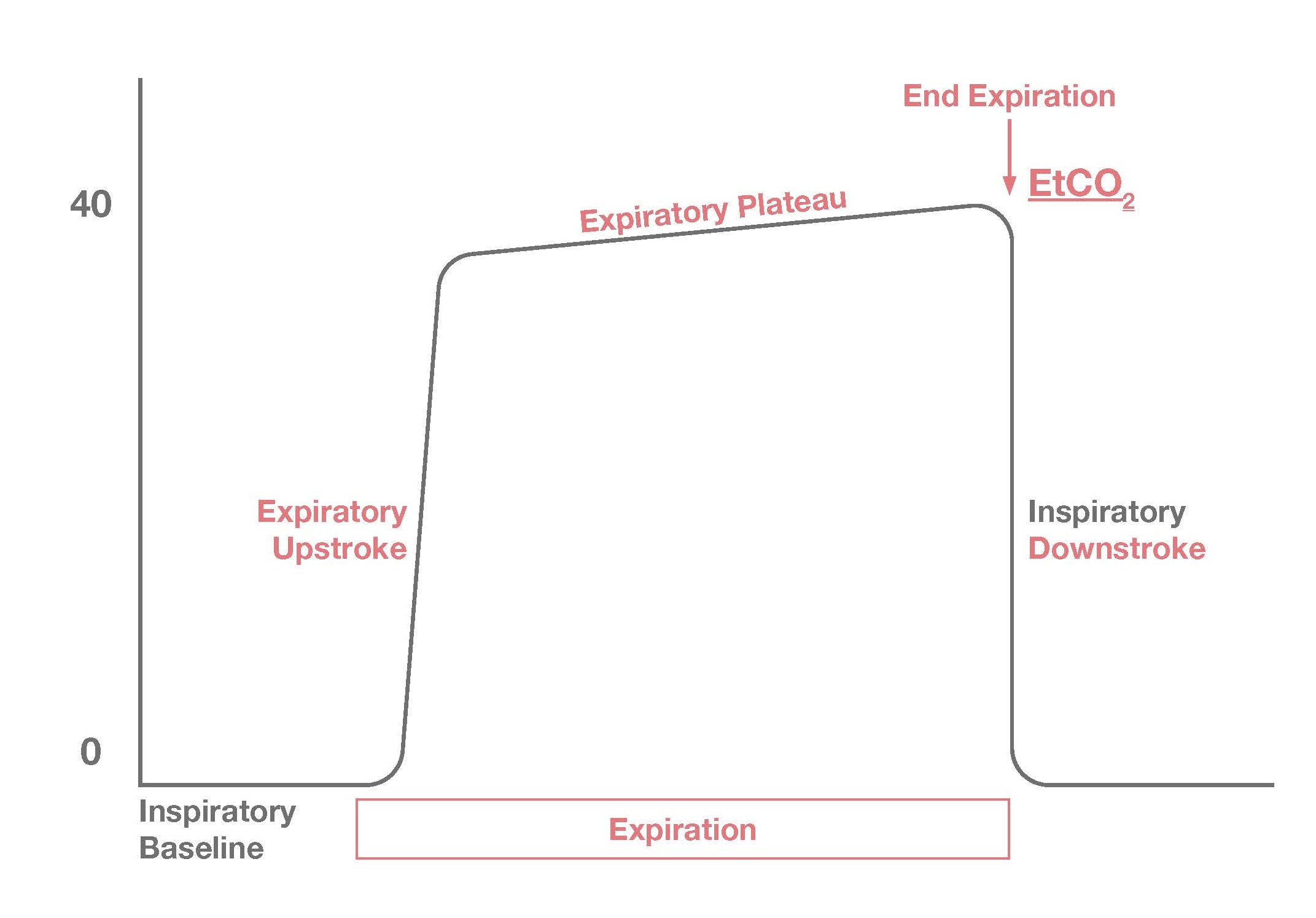
Quantitative waveform capnography is the continuous measurement of carbon dioxide (CO2), specifically end-tidal CO2. The capnography device uses a sensor that detects CO2 levels in expired air. This device can be part of a nasal cannula filter line or be attached to a bag mask device or ET tube. Of course, when a patient is being ventilated either a rescuer or a ventilator machine is assisting those expirations. This is precisely why quantitative waveform capnography is useful in life support situations.
Why do we produce carbon dioxide?
CO2 is a product of cellular respiration. As cells create energy, they consume oxygen and give off CO2 as a waste product. Therefore, if we can detect CO2 in exhaled breath it provides us with some very important information about our life support efforts. It means that:
• Cellular respiration is taking place
• That the ventilation is being delivered
• That we are creating some form of circulation
If cardiac output is insufficient, carbon dioxide returning from the tissues through the veins is not reaching the lungs. The capnography device can also provide the means of quantifying respiration rate that is more accurate than simply counting ventilations. Specifically, if the rescuer is delivering ventilations but the end-tidal carbon dioxide is too low, then ventilation is insufficient and these should not be considered actual ventilations.
Am I delivering adequate CPR?
Normal end-tidal carbon dioxide (ETCO2) usually falls in the range of 35 to 45 mmHg in adults. In an unconscious patient or in someone who is in cardiopulmonary arrest, ETCO2 may be undetectable. Rescuers should strive to deliver high-quality chest compressions that keep ETCO2 levels at least 10 mmHg and preferably 20 mmHg or higher.
If the rescuer began the intervention by delivering high-quality compressions and achieving satisfactory ETCO2 but CO2 levels dropped over time, it’s important to consider whether rescuer fatigue is setting in. A drop-in ETCO2 may prompt rescuers to switch roles and give the person delivering chest compressions a chance to recover.
Did my patients achieve ROSC?
Another use for quantitative waveform capnography is to identify patients who have achieved a return of spontaneous circulation or ROSC. Even under the best circumstances, it will be rare for a person delivering CPR to achieve 35 to 45 mmHg of ETCO2. So, if during the course of advanced cardiovascular life support a patient’s ETCO2 increases rather dramatically (e.g., from 15 to 35 mmHg) this is consistent with the return of spontaneous circulation.
Why can’t I just use pulse oximetry?
Quantitative waveform capnography provides many details about resuscitation efforts that pulse oximetry cannot. Moreover, pulse oximetry is a delayed assessment of the patient’s oxygenation status. The detection system used in pulse oximetry is slow to respond to changes in the oxygen levels of blood. Quantitative waveform capnography, on the other hand, immediately responds to changes in the level of CO2 in expired air. Therefore, it provides a real-time monitor for apnea and an assessment of effectiveness of cardiopulmonary resuscitation.
Quantitative waveform capnography provides vital insight into a patient’s ventilation and resuscitation status. Learn how to interpret and apply this life-saving monitoring tool through our online ACLS certification program.