A 55 year old man is brought in by EMS for altered mental status.
It is the middle of February and he was found sleeping outside. He smells of alcohol, is moaning on the gurney, and responds to painful stimuli.
Vital signs are assessed.
- RR: 13
- HR: 38
- BP: 110/90
- Temp: Cold to touch
- SpO2: Unable to obtain reading
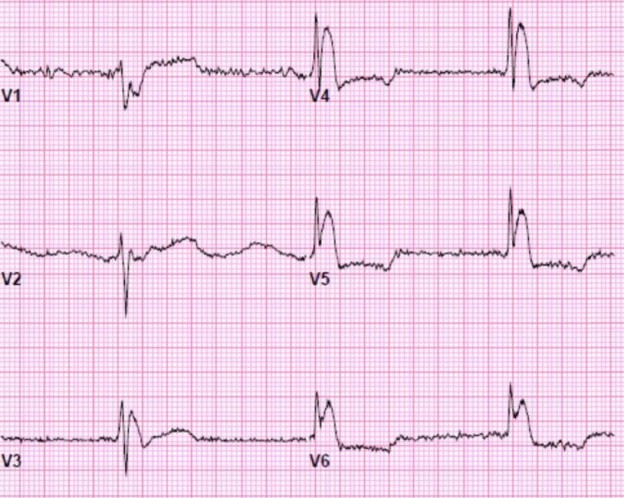
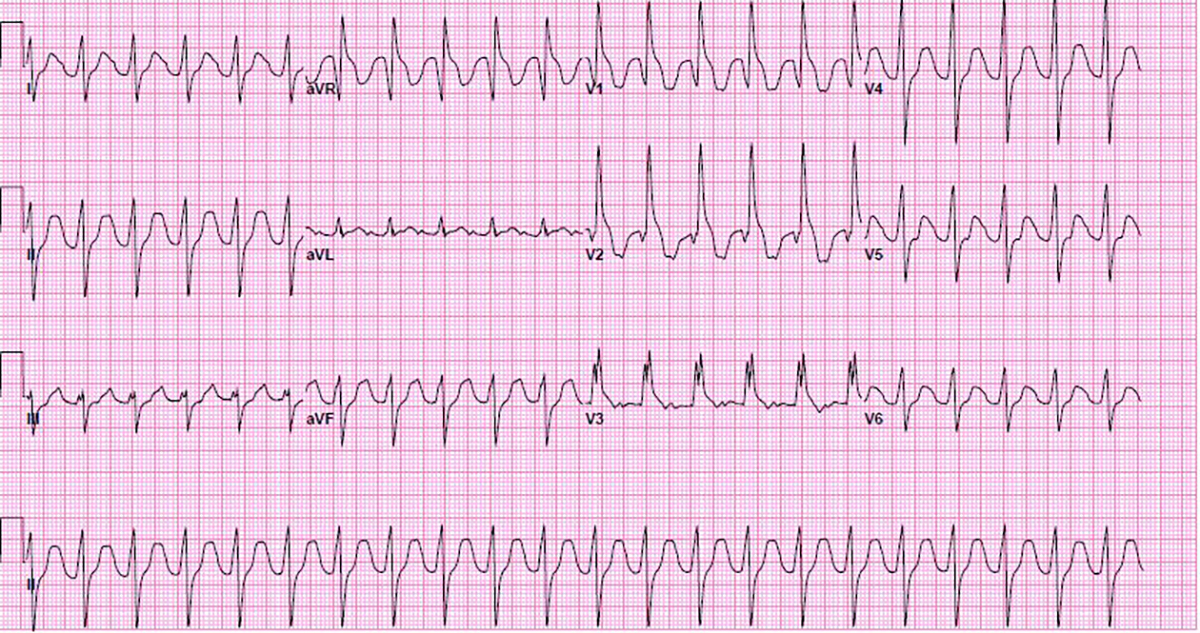
A 12-lead ECG is obtained due to bradycardia and altered mental status.

Sinus bradycardia with a rate of 38. The QRS appears to be wide and there is a large notch or J-wave at the end of the QRS complex. These are classic “Osborn waves” of hypothermia. There is motion artifact due to slight shivering.
At this point the patient’s temperature was found to be 24°C / 75°F by bladder temperature monitoring.
Osborn waves typically have a positive deflection in all leads except aVR and V1. They are known by a number of other names such as the camel-hump sign, late delta waves, hypothermic waves, or prominent J-waves.
In a patient who was found outside in February, they can safely be presumed to represent hypothermia.
The physiologic cause of Osborn waves is not well understood. Since the 1920s many hypothesis have been proposed including anoxia, injury current, acidosis, delayed ventricular depolarization and early ventricular repolarization.
While the treatment of the patient with prominent Osborn waves is based on the precipitating cause, the presence of Osborn waves is related to an increased incidence of ventricular fibrillation.
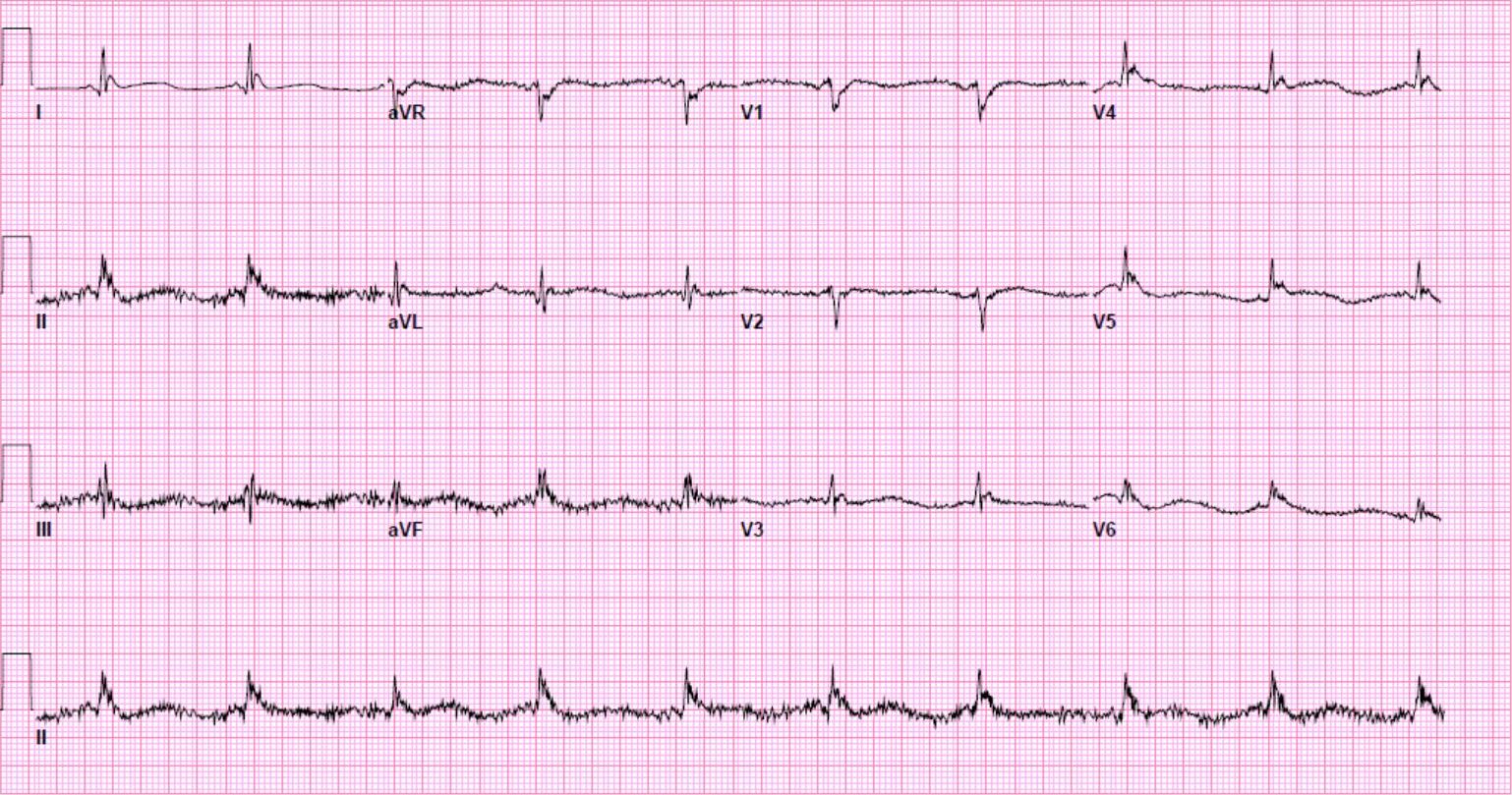
The patient was aggressively resuscitated with both internal and external warming with warm intravenous fluids and forced heated air blankets.
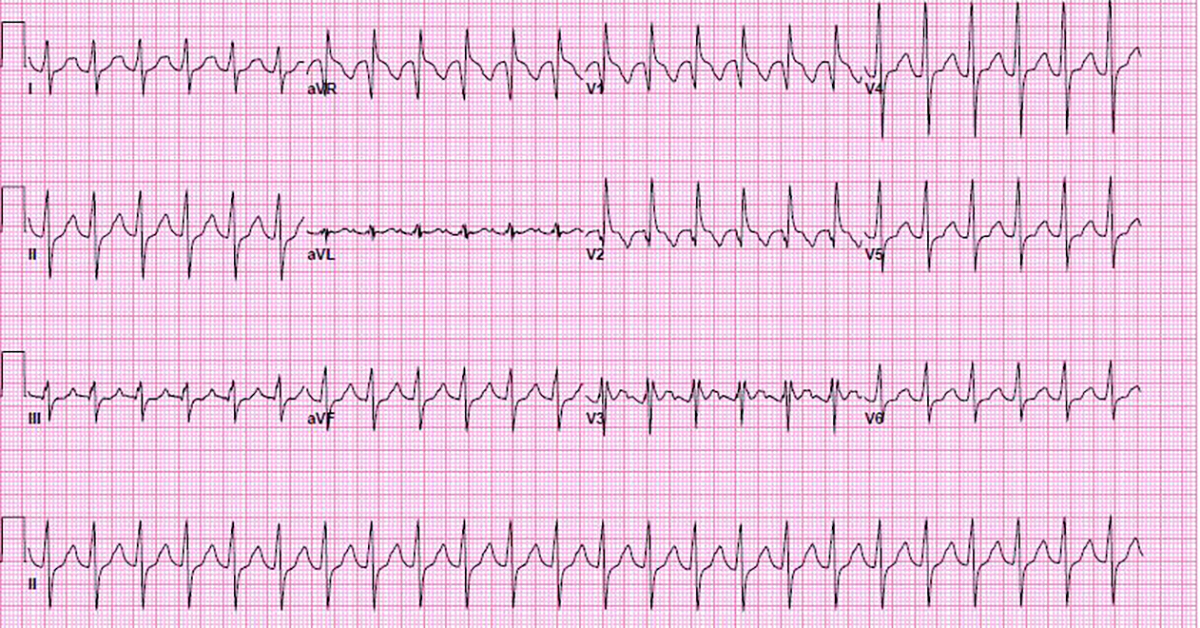
A repeat 12-lead ECG was performed 2 hours later.
The patient’s temperature is now 32°C / 89°F.
As the internal temperature improved the patient’s heart rate began to rise and the Osborn waves became less prominent. However, the artifact is worse due to increased shivering.
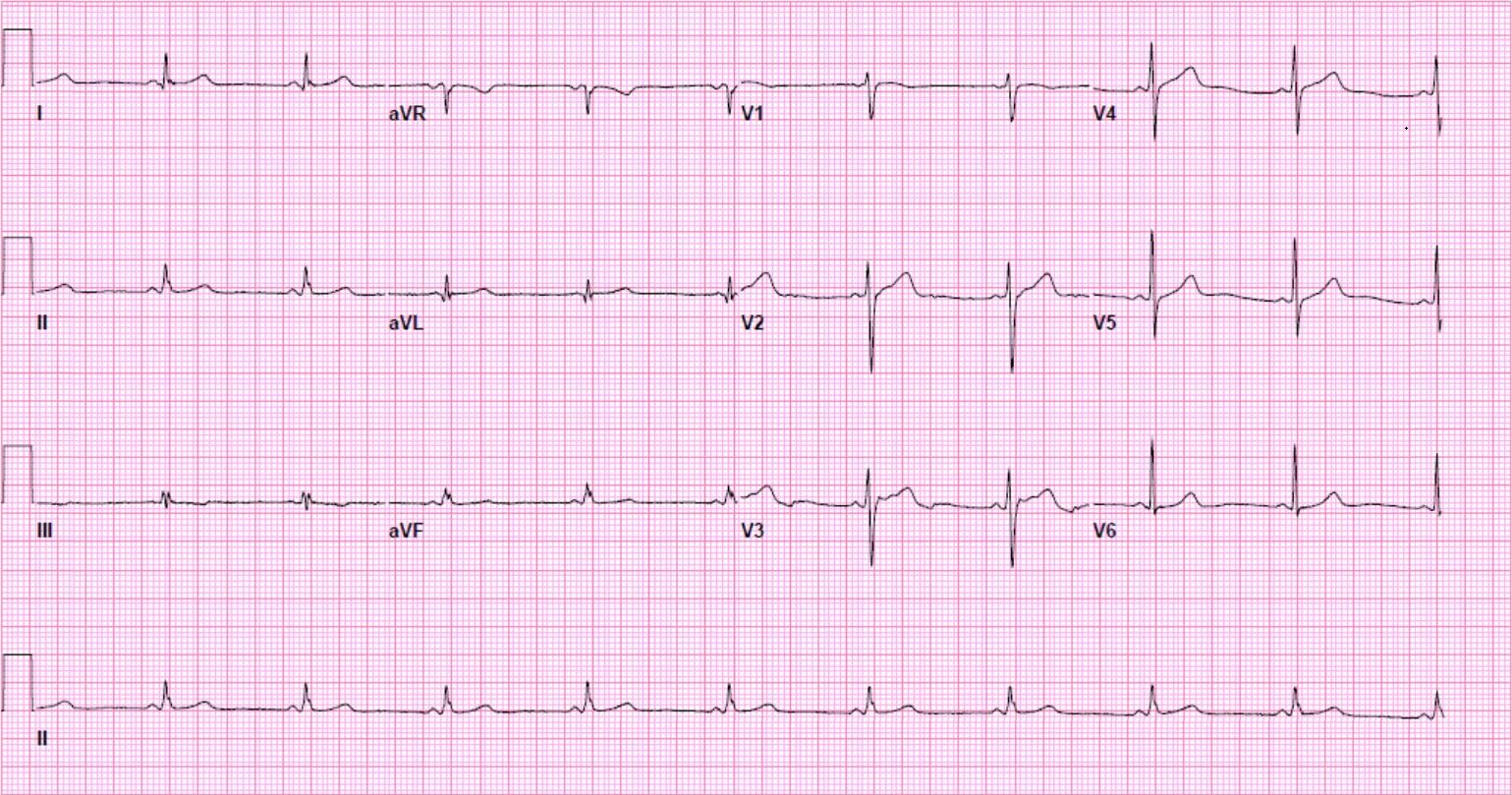
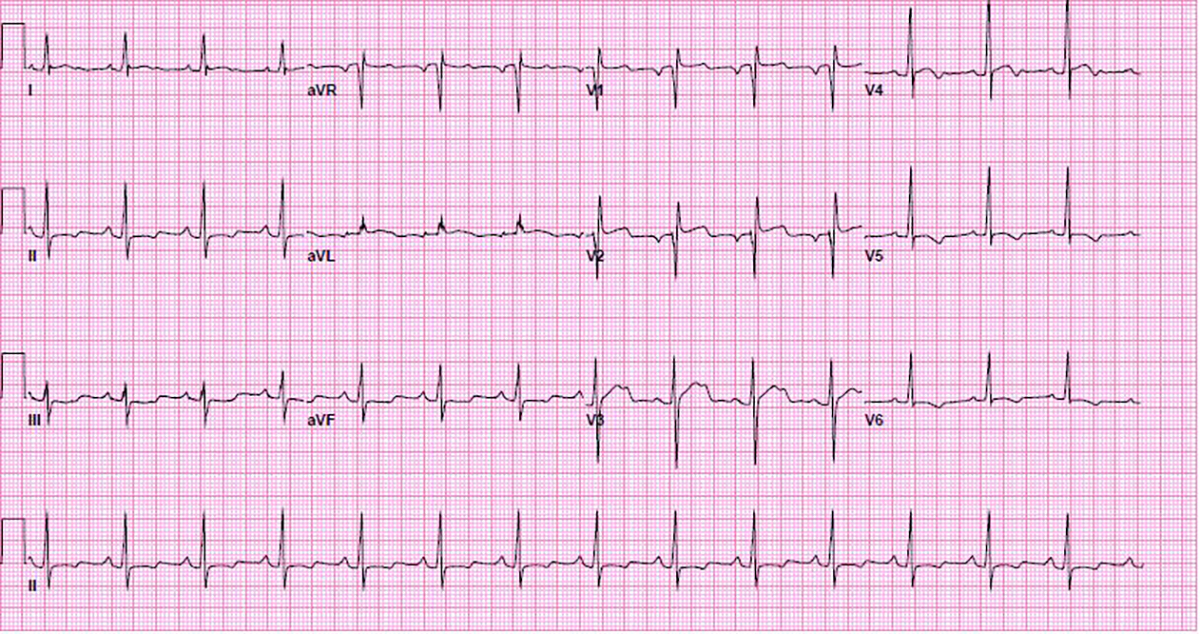
Rewarming was continued and a third ECG was performed, 3 hours after initial presentation.
Core temperature at this point was 33°C / 91°F.
Discussion
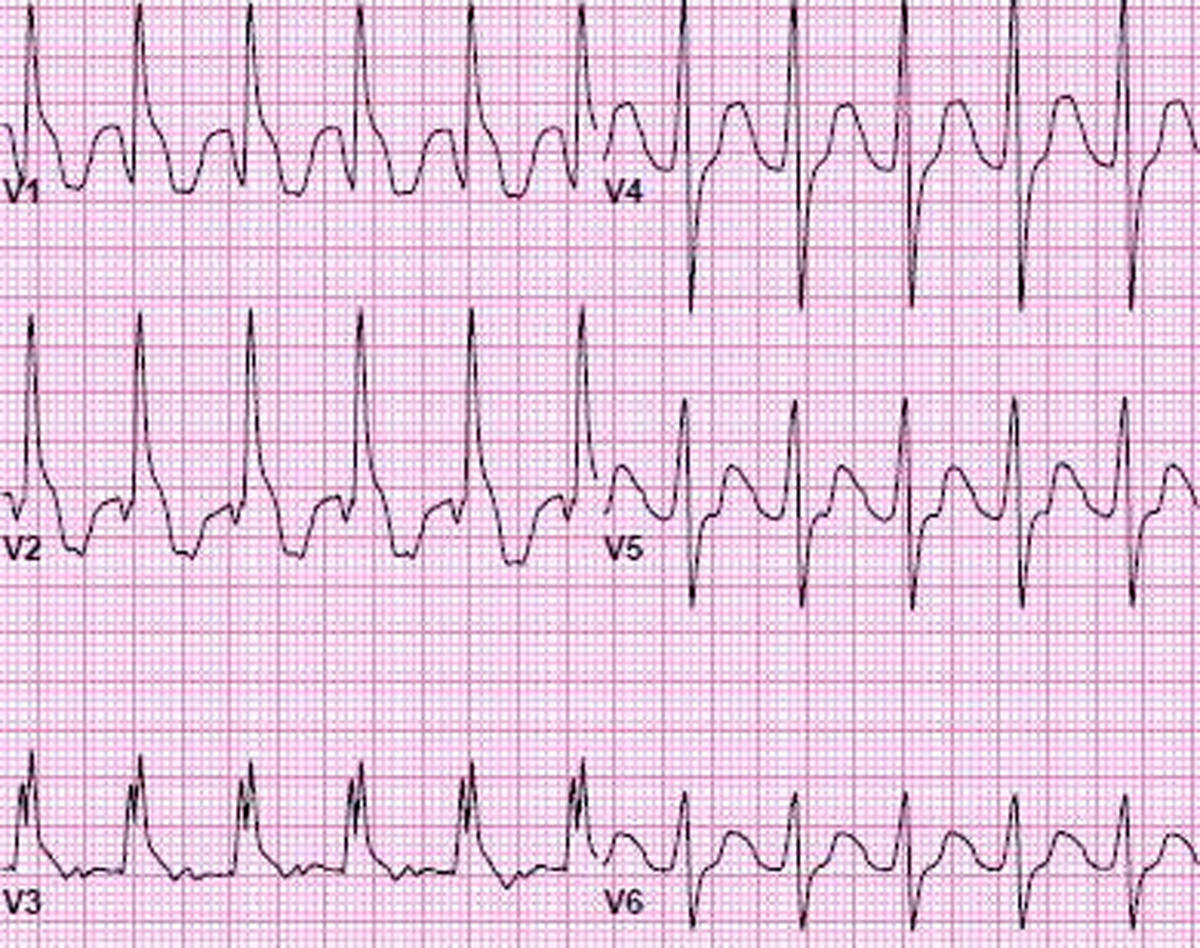
Osborn waves consist of a positive deflection at the J-point in all leads except for aVR and V1 where the deflection is negative.
Prominent J-waves can be seen in hypothermia, hypercalcemia, neurovascular accident, vasospastic angina, and Le syndrome d’Haïssaguerre (idiopathic ventricular fibrillation or as a normal variant).
While the true physiologic cause of Osborn waves is not known their presence can indicate a progression to ventricular fibrillation.
Osborn waves that are secondary to hypothermia should improve with patient warming.
Hypothermia also causes bradycardia, prolonged PR, QRS and QTc intervals, ventricular ectopy and atrial fibrillation.
Shivering may contribute to poor 12-lead ECG data quality but usually disappears below a threshold temperature.
Resources
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1501063
http://lifeinthefastlane.com/ecg-library/basics/hypothermia
http://hqmeded-ecg.blogspot.com/2011/11/osborn-waves-and-hypothermia.html